A Case Series of Sleep Bruxism Treated With Nasal Continuous Positive Airway Pressure: Craniofacial Feature and Polysomnographic Findings
Article information
Abstract
Sleep bruxism (SB) is a common disorder that presents as repetitive jaw muscle activity with clenching or grinding of teeth and/or bracing or thrusting of the mandible. Several studies have suggested that SB is associated with obstructive sleep apnea (OSA). However, the effect of treatment with continuous positive airway pressure (CPAP) on SB concomitant with OSA has not been well recognized, except in a few reported cases. Herein, we present three cases of SB with various OSA severities that were successfully treated with CPAP, as indicated by the improvement in their clinical symptoms and bruxism index on polysomnography. Our results suggest that clinicians should raise suspicion of OSA in patients with SB and be aware that patients with SB and concomitant moderate-to-severe OSA can be successfully treated with CPAP.
INTRODUCTION
Sleep bruxism (SB) is a relatively common disorder characterized by stereotyped movements, including repetitive jaw muscle activity induced by clenching or grinding of teeth and/or bracing or thrusting of the mandible [1]. According to the International Classification of Sleep Disorders (ICSD-3), SB is clinically diagnosed by regular or frequent tooth grinding sounds during sleep and the presence of one of the following clinical symptoms: 1) abnormal tooth wear consistent with the above reports of tooth grinding during sleep; 2) transient morning jaw-muscle pain or fatigue, temporal headache, and/or jaw locking upon awakening consistent with the above reports of tooth grinding during sleep [1,2]. According to an international consensus on the definition of SB, it can be graded into three types: possible SB, based on self-report; probable SB, based on clinical examination as well as self-report; and definite SB, which requires confirmation by polysomnography (PSG), a gold standard test to diagnose SB, along with self-report and clinical examination [1].
Although various etiologic factors of SB have been reported, the pathophysiological mechanism of SB remains unclear and poorly understood [3]. Previous studies have supported the notion that SB is related to autonomic and central nervous reflexes following cortical arousal [3,4]. Because obstructive sleep apnea (OSA) causes cortical arousal during sleep, it has been indicated as a new risk factor for SB [4].
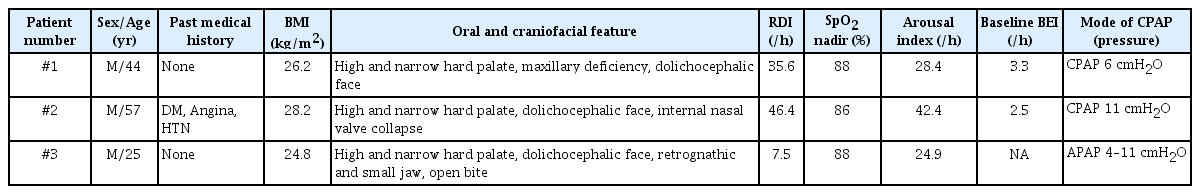
Traditionally, therapeutic modalities for SB include behavioral strategies, intraoral flat appliances, medications, and botulinum toxin injections, which are applied to reduce SB symptoms rather than treating etiologic factors [5]. As SB commonly occurs following cortical arousal after respiratory events, several previous studies have suggested that preventing respiratory events would improve SB by reducing cortical arousal [4,6]. Several case reports and clinical studies have reported the clinical utility of continuous positive airway pressure (CPAP) as a new therapeutic modality for treating SB in patients with OSA [6,7]. However, no detailed case descriptions, including craniofacial structure information of patients with SB and long-term clinical courses, have been reported. Here, we present three cases of probable SB with OSA and similar facial morphology that did not respond to conventional treatments but were treated successfully with CPAP (Table 1).
CASE REPORT
Case 1
A 44-year-old man presented to the sleep clinic with SB and morning jaw pain since nine years. He was aware of his SB and snoring, which awakened him several times at night. He underwent conventional bruxism management, including several maxillary occlusal splints; however, it did not improve SB. He had no relevant medical history and was not taking any medications. His body mass index (BMI) was 26.2 kg/m2 (177 cm, 82 kg). He had a high and narrow hard palate with a maxillary deficiency and a dolichocephalic profile (Fig. 1A). On temporomandibular examination, palpation of both masticatory muscles and joint sounds were negative. The patient exhibited a prominent scalloped tongue. The teeth were flattened and worn out because of the chronic bruxism. His Mallampati grade was 3 and neck circumference was 43 cm.

Oral and craniofacial features of patients. A: Case 1 patient exhibited a high and narrow hard palate with maxillary deficiency. On craniofacial features, he also presented a dolichocephalic profile. His teeth were flattened and worn out due to chronic bruxism. B: Case 2 patient showed a high and narrow hard palate. He had a dolichocephalic face, and internal nasal valve collapse. C: Case 3 patient had a high and narrow hard palate and open bite on oral examination. He showed a dolichocephalic face, and small and retrognathic jaw.
In-lab night PSG was performed and scored according to the guidelines of the American Academy of Sleep Medicine (AASM) [8]. SB was recorded by chin electromyography (EMG) on the submentalis muscle, and the collected data was analyzed by a trained sleep specialist/neurologist (H-R.S). Bruxism was defined when chin EMG activity was more than twice the amplitude of background EMG, and the same episode was not separated by more than 3 s [8,9]. The Bruxism episode index (BEI) was defined by the number of bruxism episodes per hour [8,9]. Over a total sleep time (TST) of 378.0 min, PSG showed severe OSA with an apnea-hypopnea index (AHI) of 33.5/h and respiratory disturbance index (RDI) of 35.6/h with heavy snoring. There were 29 episodes of bruxism, and BEI was 3.3/h. Bruxism followed the respiratory events accompanied by cortical arousal (Fig. 2A).

Night polysomnographic finding of sleep apnea and bruxism without and with nasal continuous positive airway pressure (CPAP) treatment. A: Case 1 patient showed severe obstructive sleep apnea (OSA) with an apnea-hypopnea index (AHI) of 33.5/h. with 29 episodes of bruxism (bruxism episode index [BEI] 3.3/h) following respiratory events. Sleep stages were N1 and N2. B: On full-night CPAP titration, bruxism was improved with a BEI of 1.8/h. Especially on CPAP pressure 6 cmH2O, BEI was 1.1/h. The sleep stage was N2. C: On diagnostic polysomnography, the case 2 patient presented severe OSA with an AHI of 44.7/h with a BEI of 2.5/h. The sleep stage was N1. D: During the split night CPAP titration study, the case 2 patient showed a BEI of 0.8/h, and with CPAP pressure 11 cmH2O, bruxism was resolved. The sleep stage was N1.
Treatment with auto-positive airway pressure eliminated respiratory events, markedly improved tooth grinding and jaw pain, and even reduced SB, as reported by the patient’s wife. In-laboratory CPAP titration was performed to treat the remnant SB. In the CPAP titration study, 14 episodes of SB were observed with a BEI of 1.8/h (Fig. 2B) over 479.5 min of TST. At a CPAP pressure of 6 cmH2O, no respiratory events were noted, and there were six episodes of bruxism (BEI 1.1/h). The patient was eventually switched to nasal CPAP with 6 cmH2O pressure, which he has been using consistently without any episodes of bruxism for five years.
Case 2
A 57-year-old man with a history of angina, diabetes, and hypertension presented to the sleep clinic with SB and heavy snoring since 30 years. He awoke frequently because of tooth grinding and experienced jaw fatigue and headache in the morning. His BMI was 28.2 kg/m2. Except for hypertrophy of both the masseter and temporalis muscles, temporomandibular evaluation did not reveal any abnormalities.
Physical examination revealed a high and narrow hard palate, dolichocephalic face, and internal nasal valve collapse (Fig. 1B). His teeth were worn out because of the chronic bruxism. His tongue was scalloped bilaterally, Mallampati grade was 4, and neck circumference was 43 cm.
In-lab PSG with split-night CPAP titration was performed. Over a TST of 145.0 min, diagnostic PSG revealed severe OSA with an AHI of 44.7/h, RDI of 46.4/h with heavy snoring, and six episodes of bruxism with a BEI of 2.5/h (Fig. 2C). During the split-night CPAP titration study, there were three episodes of bruxism (BEI 0.8/h), and at a CPAP pressure of 11 cmH2O, the RDI was 2.7/h without bruxism (Fig. 2D).
With a CPAP pressure of 11 cmH2O, his snoring markedly improved, as did his jaw pain and teeth grinding. However, because of remnant SB, the patient was referred to a dentist. On dental examination, two mandibular second molars (#37 and #47) were missing, and chronic periodontitis was noted. After periodontal treatment, an implant was inserted to replace the missing teeth, and botulinum toxin injection (Onabotulinumtoxin A 100 units/vial, Botox®, Allergan, Dublin, Ireland) was administered to the masticatory muscles. In addition, a mandibular advancement device (MAD) (SomnoMed, SomnoMed Ltd., Sydney, Austrailia; adjustable, two pieces) was inserted, and his quality of sleep and jaw pain improved. He is currently using MAD with CPAP without any further episodes of SB.
Case 3
A 25-year-old man visited the sleep clinic complaining of clenching and grinding of his teeth during sleep since two years. He awoke several times because of his teeth clenching. His teeth were fractured due to severe bruxism. He experienced jaw pain and toothache in the morning. He took sedative medication initially, which did not resolve the symptoms, and then tried a flat oral appliance during the night; however, this resulted in a malocclusion. He then started to undergo MAD (SomnoMed Ltd.) after consultation with a dentist, but the jaw pain worsened.
He had no relevant medical history and was not taking any medication. His BMI was 24.8 kg/m2. On physical examination, temporomandibular disorder was ruled out. He had a dolichocephalic face, high and narrow hard palate, small retrognathic jaw, and an open bite (Fig. 1C). His tongue and oral mucosa showed dental impressions owing to severe clenching. His Mallampati grade was 3 and neck circumference was 37 cm.
Over a TST of 354.0 minutes, night PSG showed mild OSA with an AHI of 5.8/h and RDI of 7.5/h, with moderate snoring. SB was not documented on nighttime PSG. Nevertheless, his symptoms met the diagnostic criteria for SB (frequent tooth grinding, abnormal tooth wear, and morning jaw pain), and was therefore diagnosed with probable SB and mild OSA.
Although sleep apnea was mild, auto CPAP was initiated. After using CPAP for one month, bruxism and clenching were greatly improved. The morning jaw pain was relieved while using CPAP, but recurred when it was not used. However, the patient discontinued the use of CPAP because of discomfort while wearing it.
DISCUSSION
The diagnosis and improvement of SB by CPAP was well documented by both diagnostic and CPAP titration PSG in the first two cases, although the third patient showed significant clinical improvement. Several reports have demonstrated a relationship between SB and sleep-disordered breathing, although this remains debatable[4,6]. It is well known that SB commonly occurs following cortical arousal after respiratory events [4]. SB may serve as a reactive and protective mechanism against upper airway obstruction [4]. This explains the temporal relationship between SB and respiratory events. In addition, there is increasing evidence that hypoxia may also play a role in causing SB [10]. A previous study showed that transient hypoxia is related to the onset of a bruxism episode, independent of arousal or body movements [10]. This relationship supports that bruxism could be improved with OSA treatment, including CPAP, by preventing transient hypoxia events.
However, another study showed that respiratory events appear to be more related to other types of sleep oromotor activity than SB, suggesting that other factors would play a role in the causation of SB [4,10]. The present cases showed similar craniofacial structures, including maxillary deficiency, high and narrow hard palate, and dolichocephalic face, suggesting that the common risk factors of SB concomitant with OSA may involve specific craniofacial morphologies. Despite the significant improvement in SB by CPAP, residual SB may persist which would require further treatment, as in the second case, suggesting that complex factors are associated with SB.
This study has some limitations. Chin EMG channel with submentalis muscle recording was only used in this study, which is not considered sufficient for definite scoring of SB episodes [1]. However, video-audio recording showed a temporal relationship between respiratory events and SB. A recent study suggested that PSG with the bilateral temporalis or masseter muscles, or both, is valid for SB recording [7]. Although SB was not confirmed by PSG in Case 3, he had a clear history of SB and reported clinical improvement of SB and related jaw pain by CPAP, suggesting that CPAP can also be used as an alternative even in probable SB, which has not been proven in PSG.
A recent study on OSA concomitant with SB showed that CPAP was as effective as MAD in reducing bruxism and more effective in reducing respiratory events [7]. Our cases confirm that CPAP therapy could be an essential treatment option for patients with SB and OSA, especially when the effect of oral appliance therapy is inadequate. In addition, the common craniofacial features among our patients, such as dolichocephalic face and a high palate, suggest that CPAP could be effective, especially in patients with these craniofacial features. A further large prospective study including mild to severe OSA with SB is needed to evaluate the risk factors for SB concomitant with OSA and the predictive factors for the response of SB to CPAP treatment.
Notes
Ethics Statement
This study adhered to the principles of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Dankook University Hospital (IRB: 2022-11-037). The requirement for informed consent was waived by IRB and all patient information was sufficiently anonymized.
Availability of Data and Material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the study.
Hye-Rim Shin and Jee Hyun Kim, contributing editors of the Journal of Sleep Medicine, were not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Hye-Rim Shin, Jee Hyun Kim. Data curation: Hye-Rim Shin, Hye-Kyoung Kim. Formal analysis: Hye-Rim Shin, Jee Hyun Kim. Supervision: Jee Hyun Kim. Visualization: Hye-Rim Shin. Writing—original draft: Hye-Rim Shin, Hye-Kyoung Kim. Writing—review & editing: all authors.
Funding Statement
None