Objective Sleep Quality in Subjects with Restless Legs Syndrome versus with Psychophysiological Insomnia: Polysomnography and Cardiopulmonary Coupling Analysis
Article information
Abstract
Objectives:
To compare the sleep quality in the view of polysomnography (PSG) and cardiopulmonary coupling (CPC) analysis in subjects with restless legs syndrome (RLS) versus with psychophysiological insomnia (PPI).
Methods
The PSG data of 109 subjects with RLS and 86 with PPI (apnea-hypopnea index <5/h) were collected. All subjects reported sleep onset and maintenance insomnia. CPC parameters were obtained using CPC analyzer in RemLogic. Sleep spectrogram by CPC analyses categorized sleep as “stable” [high-frequency coupling (HFC), 0.1–0.4 Hz] and “unstable” [low-frequency coupling (LFC), 0.1–0.01 Hz], independent of sleep stages. We compared PSG and CPC parameters between two groups and performed correlation analyses to find the PSG parameters to affect CPC parameters.
Results
In PSG parameters, subjects with PPI showed significantly longer sleep latency (14.2±20.06 vs. 27.5±34.96, p<0.001), and decreased sleep efficiency (SE, 80.5±14.96 vs. 76.5±14.45, p=0.009) than RLS. CPC parameters were not significantly different between groups. In both groups HFC was positively correlated with total sleep time and SE and was negatively associated with time of wake after sleep onset in both groups. Meanwhile, very LFC showed the opposite results to HFC with the same PSG parameters.
Conclusions
Although subjects with RLS or PPI present sleep onset and maintenance insomnia, objective sleep quality was worse in PPI than RLS. It suggests that CPC as a factor to differentiate sleep quality between the RLS and the PPI has a limited role.
Introduction
Recent test methods are seeking simplification and convenience. Conventional inspection tools are still showing magnificence in diagnosis and simple equipment is not sufficient to replace them yet. More and more simple and convenient devices have been developed with improving concordance with standard tests. Overnight polysomnography (PSG) is essential to assess the number of events occurring during sleep and to evaluate the quality of sleep. On the while, standard PSG is expensive and subjects feel inconvenience due to the large number of electrodes and wires that are attached to head and body. In addition, PSG needs appropriate facilities for tests. Cardiopulmonary coupling (CPC) analysis uses a single-channel electrocardiography (ECG) recording to extract signal features modulated by breathing [1]. Enhanced quantitative assessments of sleep quality, especially if measurable in a simple and inexpensive method, may have substantial clinical utility.
Restless legs syndrome (RLS) and psychophysiological insomnia (PPI) are sleep disorders representing sleep-onset and maintenance insomnia in common. Even if it could be distinguished by a detailed history and the thorough disease-specific questionnaires, PSG needs to detect the events that cause arousals and determine the treatment policy of subjects.
The aim of this study was to investigate objective sleep quality by the means of PSG and by CPC analyses, the utility of an operator-independent and automated measure of sleep physiology, to characterize two distinct sleep disorders.
Methods
Subjects
This is a retrospective study of RLS and PPI subjects who visited sleep center from October, 2008 to August, 2014. We excluded 261 subjects who had obstructive sleep apnea syndrome with an apnea-hypopnea index ≥5 per hour or insufficient CPC data among total 456 subjects. One hundred-ninety five subjects (age 20–70 y) were finally included in this study. Among them, 109 subjects were diagnosed as RLS and 86 subjects were to have PPI (Fig. 1). Diagnosis of RLS was based on the IRLSSG diagnostic criteria [2]. Subjects with PPI were eligible for inclusion in this study if they met the diagnosis criteria according to the International Classification of the Sleep Disorder-II criteria [3]. Subjective daytime sleepiness was measured by the Epworth Sleepiness Scale (ESS) and Stanford sleepiness scale. The severity of RLS was scored by the International Restless Legs scale (IRLS) [4]. All subjects were evaluated with overnight PSG and we extracted the CPC parameters from single ECG signal from each PSG data to estimate the sleep quality.
Overnight polysomnography
Sleep studies were performed by Embla N7000 & RemLogic (Embla Systems, Denver, CO, USA). The determination of sleep stage and arousal was measured by electroencephalogram (EEG, C3-A2, C4-A1, O1-A2, O2-A1), bilateral electrooculograms and chin electromyogram. Other devices included things like chest and abdominal excursion by piezo bands, finger pulse oximetry, single-lead ECG in the modified V2 lead, bilateral leg electromyograms, snoring by pre-tracheal microphone, and body position. Airflow was monitored with thermistors and nasal-cannula pressure transducer during diagnostic sleep studies. Sleep and arousal scoring were performed using standard criteria. The PSG were scored for sleep and sleep-disorders breathing events using the 2007 guidelines of the American Academy of Sleep Medicine [5-7]. From these measures, amounts of each sleep stage, latency to each sleep stage, total sleep time (TST), sleep efficiency (SE), and wake after sleep onset (WASO) were all calculated.
Cardiopulmonary coupling analysis
Cardiopulmonary coupling analysis was performed on the single channel ECG data extracted from the diagnostic PSG using available software, RemLogic CPC analyzer. It is composed of a total of five parameters: 1) high-frequency coupling (HFC, spectrogram peaks in the frequency range of 0.1–0.5 Hz), which indicates stable sleep; 2) low-frequency coupling (LFC, spectrogram peaks in the frequency range of 0.01–0.1 Hz), which indicates unstable sleep; 3) very-low-frequency coupling (vLFC, spectrogram peaks in the frequency range of 0.00391–0.01 Hz), which indicates awake or parts of stage R; 4) other (spectrogram peaks other than HFC, LFC, and vLFC, typically <1–2%); and 5) elevated low-frequency coupling (e-LFC, a subset of LFC with especially large low-frequency power), which correlates with sleep fragmentation and sleep apnea [1,8].
Statistical analysis
Statistical analyses were performed with SPSS software (SPSS 18.0, SPSS Inc., Chicago, IL, USA). The significance level was set at p value less than 0.05. Two-sample independent t-test was used to assess differences of demographics, PSG and CPC data between the RLS and the PPI group. Partial Spearman correlations between CPC parameters and PSG data in each group were applied after adjusting for age and sex.
Results
Demographics (Table 1)
There were no significant differences in age between two groups. In both groups, the proportion of female gender was predominantly higher and significantly different between groups (75.6% in PPI vs. 60.6% in RLS, p=0.032). Mean ESS values of subjects with RLS were statistically higher (7.63±4.44 in RLS vs. 5.96±4.31 in PPI, p=0.013) compared to PPI, however, in both groups, ESS scores did not indicate clinically significant sleepiness.
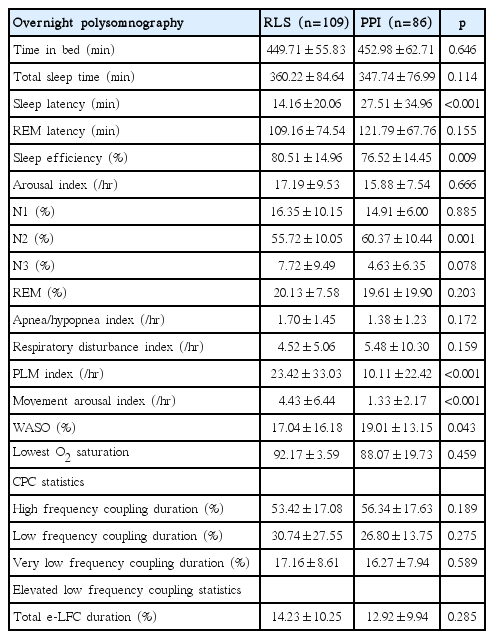
PSG and CPC parameters (Table 2)
In the PSG comparisons, subjects with PPI showed significantly extended sleep latency (14.16±20.06 vs. 27.51±34.96, p<0.001), decreased SE (80.51±14.96 vs. 76.52±14.45, p=0.009), increased N2 sleep (55.72±10.05 vs. 60.37±10.44, p=0.001), and increased WASO (17.04±16.18 vs. 19.01±13.15, p=0.043). Subjects with RLS had increased periodic limb movement index (23.42±33.03 vs. 10.11±22.42, p<0.001) and movement arousal index (4.43±6.44 vs. 1.33±2.17, p<0.001). In CPC data, there were no significant differences between two groups.
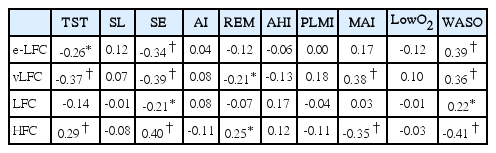
Correlation analyses between PSG parameters and CPC parameters
Subjects with RLS
In 109 subjects with RLS, after adjustment of age and gender, TST and SE were negatively correlated with e-LFC (rho=-0.26, p=0.01 and rho=-0.34, p<0.0001), vLFC (rho=-0.37, p<0.0001 and rho=-0.39, p<0.0001), LFC (rho=-0.14, p=0.15 and rho=-0.21, p=0.03) and positively correlated with HFC (rho=0.29, p<0.0001 and rho=0.40, p<0.0001). WASO was positively correlated with e-LFC (rho=0.39, p<0.0001), vLFC (rho=0.36, p<0.0001), LFC (rho=0.22, p=0.02) and negatively correlated with HFC (rho=-0.41, p<0.0001) (Table 3).
Subjects with PPI
In 86 subjects with PPI, after adjustment of age and gender, TST and SE were negatively correlated with vLFC (rho=-0.49, p<0.0001 and rho=-0.52, p<0.0001), and positively correlated with HFC (rho=0.40, p<0.0001 and rho=0.38, p<0.0001). WASO was positively correlated with e-LFC (rho=0.23, p=0.03), vLFC (rho=0.54, p<0.0001) and negatively correlated with HFC (rho=-0.42, p<0.0001) (Table 4).
Discussion
Disturbed sleep is a common, prominent, and distressing symptom in subjects with RLS or PPI. Sleep onset and maintenance insomnia-related complaints in individuals with RLS or PPI are notably higher than in controls [9]. Difficulty initiating sleep (DIS), difficulty maintaining sleep (DMS) and non-restorative sleep, have found that individuals with RLS were two to three times more likely to report these symptoms than non-RLS subjects [10,11]. The proportion of RLS individuals who reported having DIS varied from 27.9% to 69.2% and having DMS varied from 24% to 50.5% [10-12]. The PPI is characterized primarily by heightened arousal and learned sleep-preventing associations. PPI subjects usually demonstrate excessive focus on and worry about sleep and suffer from elevated levels of cognitive and somatic arousals, particularly at bedtime. In a study of 133 subjects, a large majority of RLS subjects (84.7%) experienced difficulty falling asleep at night because of RLS symptoms, and 86% reported that symptoms woke them up frequently during the night [13]. Ninety-four % reported at least one of these two manifestations.
The PSG findings of RLS subjects exhibited prolonged sleep onset latencies, shorter TST, lower SE, higher arousal index, higher number of stage shifts, and longer rapid eye movement (REM) sleep latency compared to normal controls [12]. During the sleep, percentage of wake and sleep stage 1 were increased, and sleep stage 2 and REM sleep were decreased in RLS subjects [14]. A great majority of subjects with RLS also experience stereotyped repetitive movements once asleep, a condition known as periodic limb movement during sleep (PLMS) [15,16]. PPI also show similar results except PLMS [12,17]. Current study showed a similar PSG finding to the previous researches. However PPI subjects showed significantly worse profiles of TST, SE and WASO than RLS subjects, suggesting that PPI patients were revealed to have worse sleep quality than RLS.
Respiration induces small alterations in heart rate and amplitude variations in R-wave amplitude. Using computerized frequency domain analysis, a high-frequency component can be isolated that represents variations in breathing-induced vagal sinus pressure heart rate. A low-frequency component can be extracted that provides data about interbreath intervals. In general, normal breathing loads high-frequency bands, and sleep-disordered breathing masses in low-frequency troughs [18]. Therefore, the CPC might be considered as the alternative parameters reflecting sleep quality in RLS or PPI. The situations that induce arousal or WASO increase would be related with change in the CPC parameters. Schramm et al. found that primary insomnia subjects (n=50) had lower HFC, and HFC/LFC ratio compared to the good sleepers (n=36) [19]. In this study, ewe did not find significant CPC parameters with different profiles between RLS and PPI. Both studies applied the similar methods of analysis, however, different profiles of subjects might lead different CPC results. Schramm et al. chose controls as good sleepers, while we compared two distinct sleep disorders groups presenting insomnia-related symptoms. It is plausible that CPC profiles of insomnia patients are different from normal controls since insomnia has a close link to autonomic instability before and during sleep [19]. In this study, we tried to investigate whether CPC parameters are sensitive to differentiate two sleep-disorders groups with the similar sleep-related problems. Although it failed to find significant differences in CPC parameters between two groups, it is remarkable to demonstrate that vLFC indicating unstable sleep is closely associated with SE and WASO in PSG parameters in both groups. It suggests that CPC is valuable to disclose autonomic function although it has a limited role to differentiate two distinct sleep disorders presenting similar sleep complaints.
In conclusion, RLS and PPI subjects complain of disturbed sleep and poor quality of sleep that were confirmed by PSG parameters. We expected CPC parameters to be another simple and reliable tool to characterize sleep disorders, however, we found to be insensitive to differentiate sleep quality in subjects who have autonomic dysfunction in common.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning, Republic of Korea (No. 2014R1A1A3049510) and by Samsung Biomedical Research Institute grant (#OTX0002111).